LEARN MORE
Community Resource Specialists are available between 8 a.m. to 5 p.m. M-F at (408) 350-3200, option 1.
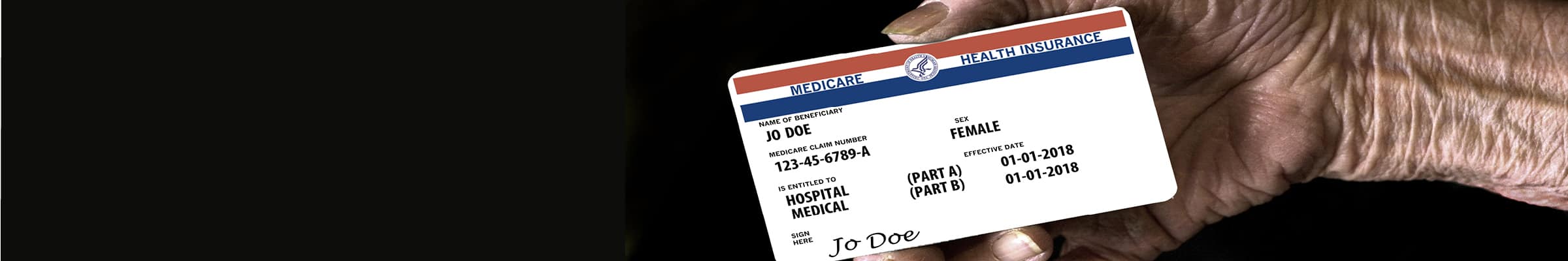
The Future of Cal MediConnect
Information for Beneficiaries
On January 1, 2023, your Cal MediConnect plan will change into a matching Medicare and Medi-Cal plan provided by the same company that provides your Cal MediConnect. These matching plans are designed to coordinate care for people with both Medicare and Medi-Cal. You will still get the same health care benefits as you do today.
You will get all your services through Cal MediConnect until December 31, 2022. Then on January 1, 2023, you will automatically start getting services through your matching plans instead. If you are in Cal MediConnect today, you do NOT need to do anything to enroll into the matching plans and keep your current benefits.
Your new plans will help you with all your health care needs and will continue to coordinate your benefits and care. This includes medical and home- and community-based services. It also includes medical supplies and medications. The matching plans will include the doctors you see today, or help you find a new doctor that you like.
You will start getting letters about this change in October 2022. You don’t have to do anything this fall to keep getting your health care from the plan you have today. If you have questions about your coverage in 2022, please contact your current Cal MediConnect plan.
Changing into Medicare Medi-Cal Plans (MMPs)
The Cal MediConnect program is transitioning on December 31, 2022. Starting on January 1, 2023, Cal MediConnect members will be transitioned to exclusively aligned enrollment (EAE) Dual Eligible Special Needs Plans (D-SNPs) and matching Medi-Cal Managed Care Plans (MCPs). Under exclusively aligned enrollment, beneficiaries can enroll in a D-SNP for Medicare benefits and in a Medi-Cal managed care plan for Medi-Cal benefits, which are both operated by the same parent organization for better care coordination and integration.
EAE D-SNPs offers an integrated approach to care and care coordination that is like Cal MediConnect. The matching Medicare and Medi-Cal plans will work together to deliver all covered benefits to their members. And as all members in the plan are also enrolled in the matching MCP, they can receive integrated member materials, such as one integrated member ID card.
The transition will happen in all Coordinated Care Initiative (CCI) counties – Los Angeles, Orange, Riverside, San Bernardino, San Diego, San Mateo, and Santa Clara. Existing Cal MediConnect plans and all Medi-Cal Managed Care Plans in these counties must create EAE D-SNPs by January 1, 2023, to support this transition.
Not sure where to begin?
For an appointment, contact our Community Resource Specialists at (408) 350-3200, option 1.
For Medicare-related questions, complete the HICAP Interest Form.

The project described was supported by Funding Opportunity Number CMS-1J1-19-001 from the U.S. Department of Health & Human Services, Centers for Medicare & Medicaid Services, Center for Medicare & Medicaid Innovation. The contents provided are solely the responsibility of the authors and do not necessarily represent the official views of HHS or any of its agencies.
Support provided by the California Department of Aging.
